HIV prevention and STI detection go hand in hand
You are here

Certain population groups are more prone to develop HIV
Human immunodeficiency virus (HIV) is a virus which weakens an individual’s immune system, potentially leading to additional infections and cancer. Due to increased access to effective prevention and improved treatment methods, the disease has become more manageable over the years, allowing HIV positive individuals to live a longer, healthier life (1).
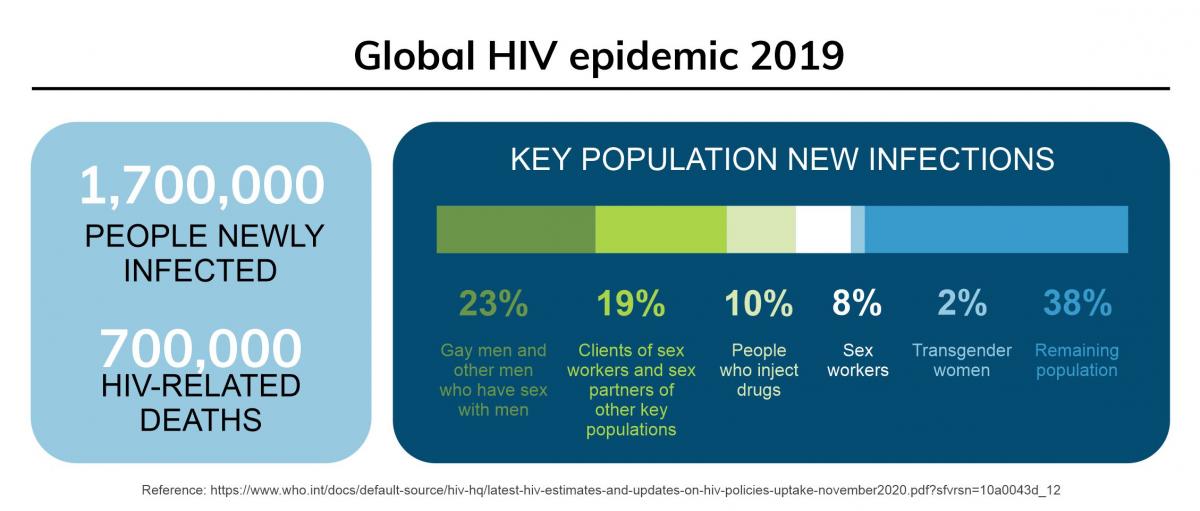
However, despite the progress, HIV continues to remain a global health issue, with an estimated 38 million people living with the disease in 2019. Certain population groups are at higher risk of acquiring HIV. Men who have sex with men (MSM), people who inject drugs, incarcerated people, sex workers, and transgender people are at increased HIV infection risk, and UNAIDS estimates that as many as 50% of all new HIV infections worldwide occur in these key groups (2).
Read our blog about the link between HIV and HPV
PrEP is highly effective at preventing HIV, but users are often also at increased risk of STIs
Pre-exposure prophylaxis (PrEP) has shown to significantly reduce risk of HIV contraction in MSM groups. When taken consistently, PrEP can lower HIV infection by more than 95% (3). Consequently, one key strategy set to end AIDS by 2030, includes scaling up the use of PrEP by uninfected persons who are more likely to acquire HIV (4).
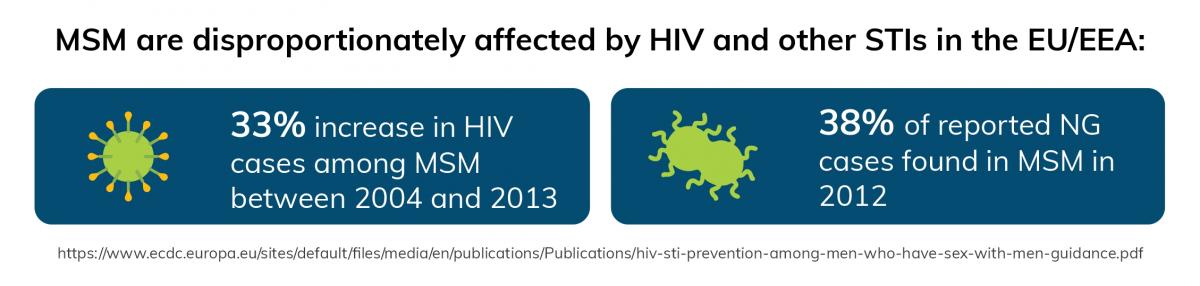
Alongside higher risk of contracting HIV, MSM and other key populations, including those initiated on PrEP, are disproportionally affected by sexually transmitted infections (STIs) such as Chlamydia trachomatis (CT), Mycoplasma genitalium (MG), Neisseria gonorrhea (NG), Trichomonas vaginalis (TV) (5).
Data in the EU/EEA shows that there was a 33% increase in HIV cases among MSM between 2004 and 2013. Further, an increase in NG cases were also reported in this region, with 38% of cases reported in MSM in 2012 (6).
PrEP provides the opportunity to reach people at highest HIV and STI risk, expanding HIV prevention and optimizing STI services
As STIs are often asymptomatic but associated with long-term morbidity, regular screening and treatment are necessary components of PrEP patient care (5). These methods are also important to decrease the STI burden in this group because of decreased condom use (7).
Regular testing of PrEP users is not only important to minimize STI infection risk at an individual level but also to eradicate relevant transmission reservoirs at a public health level (5).
The Center for Disease Control and Prevention (CDC) recommends that individuals on PrEP should undergo STI screening at least every six months when sexually active or every 3 months for those with STI signs or MSM who are at high risk (8).
Urine is a more accepted and effective sample type to detect STIs
Currently, first-void urine (20-30 mL of urine flow) is the sample of choice for the detection of CT, NG and MG in men, using nucleic acid amplification tests (NAATs). However, collecting first-void urine in a regular urine container is not standardized and can be awkward, messy and inconvenient for the user.
Novosanis’ unique urine capturing device, Colli-Pee®, allows for an easy and user-friendly collection of the first-void urine fraction.
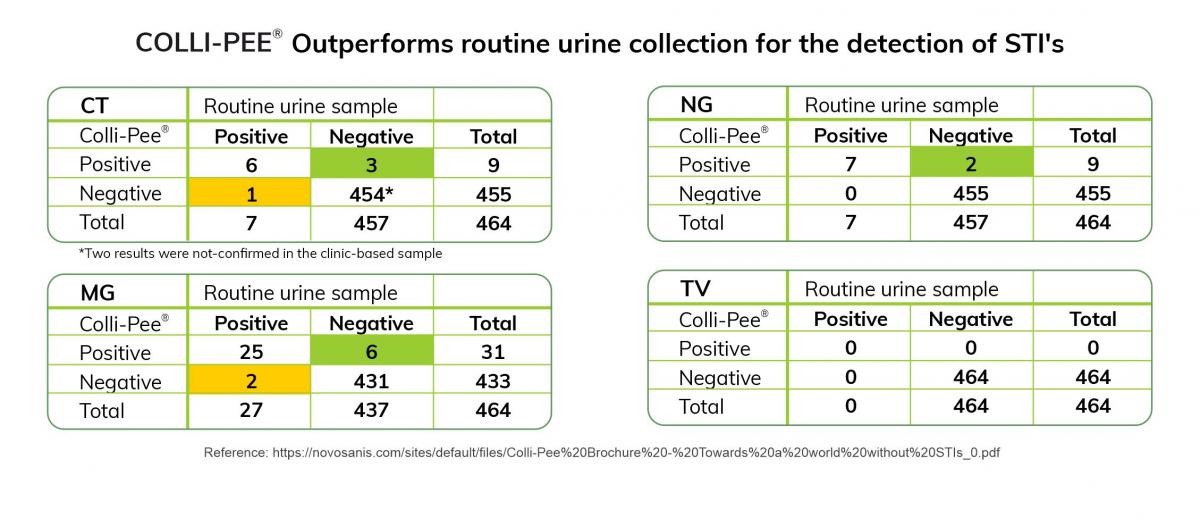
Recent research conducted by the Tropical Institute of Medicine in Antwerp, Belgium, showed that home-based collection through a first-void capturing device like Colli-Pee® positively influenced the quality of STI testing. The study compared routine clinic-based urine collection using a regular urine cup with home-collected urine samples using Colli-Pee® among MSM PrEP users. A total of 464 home-collected urine samples were analyzed and compared to their equivalent clinic-based samples at three intervals over 18 months. Only 3 infections were not detected in the home-collected urine samples, while 11 additional STIs (three CT, two NG and six MG infections) were detected in home-collected samples and not in the equivalent clinic-collected urine sample (9).
Home-based urine collection followed by postal delivery, has the potential to facilitate patient flow and allow for immediate treatment of STIs by PrEP users. It offers the ability to reach a wider population, especially any individuals at higher risk of HIV or STIs or participants that are reluctant to access traditional STI health services (9).
Conclusion
The prevalence and incidence of STIs remain high worldwide. Given the synergies between PrEP, HIV and STIs, steps are required to ensure that population groups at risk have the necessary resources to prevent infections. The World Health Organization (WHO) strongly advises PrEP users to have access to a range of services, including HIV testing, availability to male and female condoms and lubricants, opportunities to vaccinate for viral hepatitis (HAV/HBV) and Human Papillomavirus (HPV), as well as screening and treatment of STIs, among others (10). Better integration through urine sampling can allow improved STI control, as well as broaden sexual and reproductive health services, especially in groups at disproportionate risk.
References:
(1) https://www.who.int/news-room/fact-sheets/detail/hiv-aids
(2) https://www.who.int/docs/default-source/hiv-hq/latest-hiv-estimates-and-...)
(3) PMID: 28505240
(4) https://www.unaids.org/sites/default/files/media_asset/fast-track-commitments_en.pdf
(5) PMID: 32033533
(6) https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Pub...
(7) PMID: 30117076
(8) https://www.cdc.gov/hiv/effectiveinterventions/prevent/prep/index.html#:...(P WID)
(9) PMID: 30948618
(10) https://apps.who.int/iris/bitstream/handle/10665/325908/WHO-CDS-HIV-19.9...
