Urine as a way to screen more women for gynecological cancers during a pandemic and beyond
You are here
The COVID-19 pandemic has affected many sectors and industries. Healthcare services, including cancer screening have significantly dropped as a result of the situation. In the United States (US), for example, as of April 25, 2020, a 94% drop was seen in cervical cytology (1). Similarly, in the United Kingdom (UK), COVID-19 has put huge pressure on cancer services, with around 2.1 million people waiting for breast, bowel or cervical screening (1).
Finding alternative methods, which are easy, and can be followed or monitored independently, is important to continue cancer screening in these times.
We focus on two types of gynecological cancers – cervical and ovarian cancer and how urine can be used as a sample type for screening.

The problem
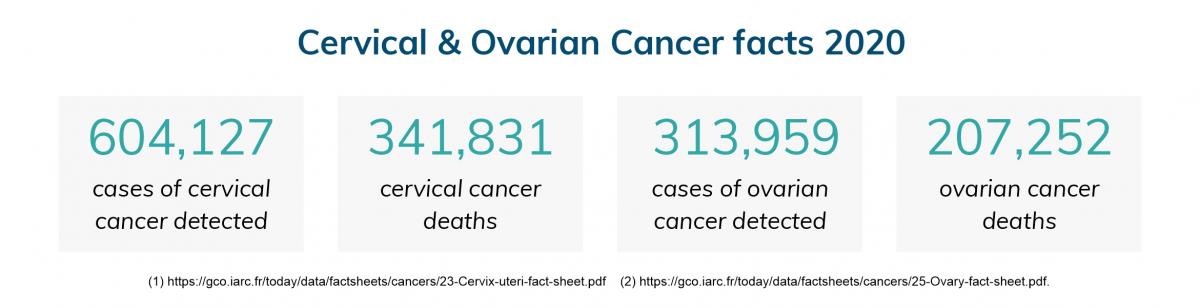
Cervical and ovarian cancer are among the top eight cancers that affect women.
Despite effective vaccination and screening programs, cervical cancer remains the fourth most common cancer type (2). Alternatively, most women present ovarian cancer at an advanced stage, making it the seventh most common malignancy among women worldwide (3).
Early detection is key
Early detection is key to improving mortality rates for both cancer types.
Cervical cancer
Despite the benefits of screening for cervical cancer, many women are often reluctant to undergo Pap smears (3). Smears are invasive and associated with physical discomfort. Lack of time or inconvenient clinic hours are also often listed as reasons why women avoid regular testing. Socials factors, including religion and culture, can also influence the decision of testing (4,5).
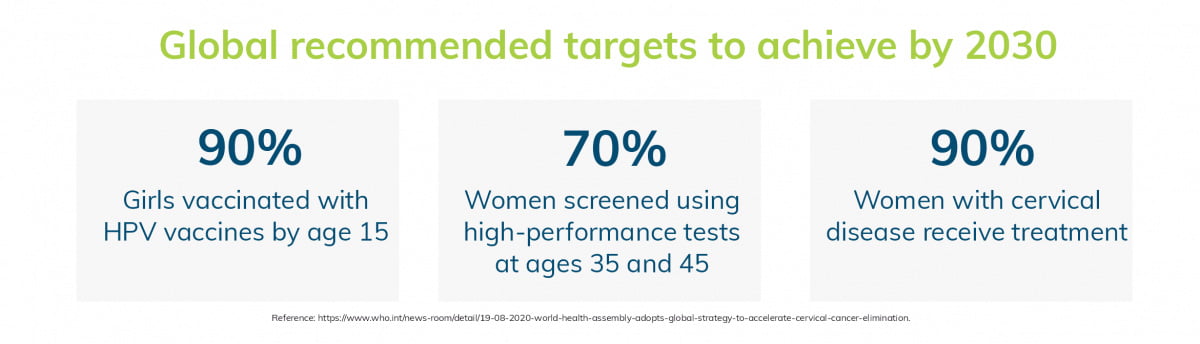
Improved screening is one key method to reach the goals set by the World Health Organization (WHO) to accelerate the elimination of cervical cancer by 2030 (6).
Ovarian cancer
Ovarian cancer is difficult to detect at an early stage due to the lack of clear symptoms and efficient diagnostic tools (7). Current methods for detection, including a pelvic examination, transvaginal ultrasonography (TVUS), blood tests to detect cancer antigen 125 (CA125), as well as surgery are perceived to be invasive, preventing many women from testing early (8).
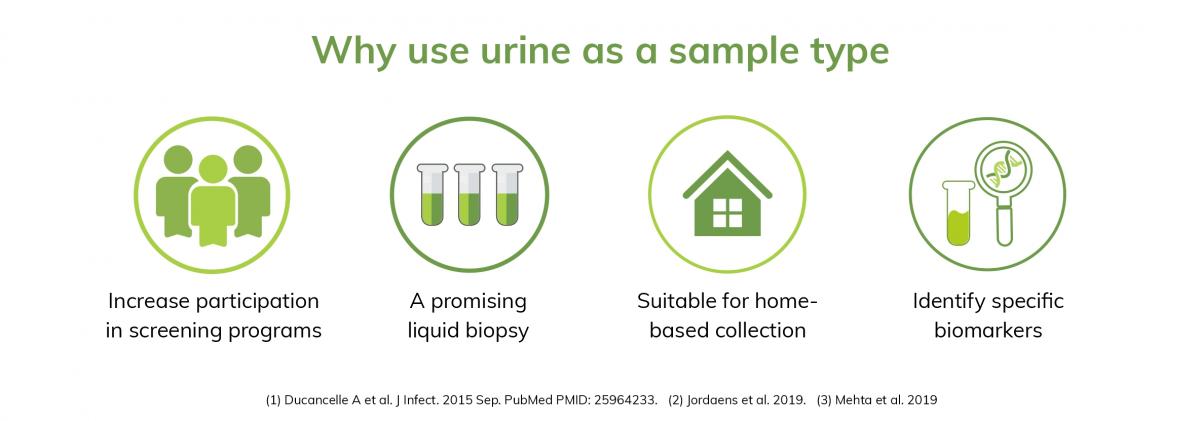
Urine can act as a potential sample type to screen more women
Given the challenges in screening, finding alternative yet effective methods, which are easy, non-invasive, to screen more women is necessary.
Cervical cancer
Most cases of cervical cancer have been linked to 14 types of high-risk Human Papillomavirus (hrHPV), a common sexually transmitted infection. Self-sampling for HPV, through brush-based techniques, or urine sampling, offers the opportunity to reach more women, especially those who do not participate in traditional screening programs (9,10).
Women have reported a significantly higher preference for urine as a sample type for hrHPV testing. Additionally, urine showed similar performance to clinician-taken smears as well as brush-based self-sampling, with almost perfect detection of HPV in women with CIN2+ (cervical intraepithelial neoplasia grade 2+) (11), emphasizing the potential of urine as a sample type.
While urine allows for HPV detection, the concentration of HPV is not the same in all urine fractions. Studies have shown that first-void urine (initial urine flow) contains higher concentrations of HPV DNA than midstream urine (12,13), highlighting the importance of collecting this fraction for improved sensitivity.
Learn more about urine as a preferred sample type for cervical cancer screening
The potential of urine as a source of biomarkers has also been investigated in ovarian cancer. While still in the early stages of research, studies have shown several biomarkers in urine, including proteins, metabolites and RNA transcripts for ovarian cancer.
Learn more about urine for ovarian cancer research
Colli-Pee as a urine collection device
https://novosanis.com/blog/urine-sampling-way-continue-cervical-cancer-s... https://www.who.int/health-topics/cervical-cancer#tab=tab_1 https://www.wcrf.org/dietandcancer/cancer-trends/ovarian-cancer-statistics PMCID: 23618210 https://www.tandfonline.com/doi/full/10.1080/21642850.2020.1798239 https://www.who.int/news-room/events/detail/2020/11/17/default-calendar/... PMID: 33086611 PMID: 30833816 PMID: 28689156 PMID: 32212991 PMID: 28391609 PMID: 28391609 PMID: 24916950 PMID: 28039447
