March 24 marks World Tuberculosis Day
You are here

Tuberculosis (TB) remains a global health problem and is one of the top ten causes of death globally (WHO, Global Tuberculosis Report, 2018).
The disease is primarily caused by Mycobacterium tuberculosis (MTB), which typically affect the lungs. Extrapulmonary TB, which develops outside the lungs, is less common. The disease affects all age groups and is spread across the world. However, over 95% of TB cases occur in developing countries - India, China, Indonesia, the Philippines, Pakistan, Nigeria, Bangladesh and South Africa accounted for the largest number of new cases in 2017 (WHO).

While the disease is preventable, many cases remain undetected. For several years, the most common test to detect the disease was through sputum smear microscopy, which involved analysis of sputum under a microscope for TB bacteria. Sputum is a mixture of saliva and mucus coughed from the respiratory tract. However, the procedure had limitations and sensitivity in clinical practice varied between 35 to 80% (Peter et. al, 2010).
Sputum cultures are another routine technique for TB detection, and monitors growth of bacteria. While the sensitivity of mycobacterial cultures is greater, the procedure can take several weeks to provide results, especially as TB bacteria are slow growing (Tavares e Castro et. al, 2015). Additionally, culture tests are expensive, require specialized laboratory facilities, which are not available in many counties, in particular, high-burden TB areas (Peter et. al, 2010).
Newer molecular technologies allow for improved TB detection and sensitivity. However molecular tests are costly and cannot be used in many testing centres due to the need of specific laboratory requirements and equipment (WHO, High-Priority Target Product Profiles For New Tuberculosis Diagnostics Report, 2014).
While sputum has been the most widely used sample type to detect TB, some target groups, such as children as well as individuals infected with human immunodeficiency virus (HIV) are not always able to provide a good quality sample (WHO, High-Priority Target Product Profiles For New Tuberculosis Diagnostics Report, 2014). For example, the sensitivity of sputum smear microscopy is reported to drop as low as 20% in TB-HIV co-infected patients, resulting in misdiagnosis and increased mortality in this subgroup. Furthermore, extrapulmonary TB is difficult to detect through sputum evaluation (Peter et. al, 2010; WHO, High-Priority Target Product Profiles For New Tuberculosis Diagnostics Report, 2014).
Given the severity of the TB epidemic and a world-wide effort to eliminate the disease by 2030 (WHO, Global Tuberculosis Report, 2018), researchers around the globe are searching for alternative, rapid, inexpensive, non-sputum-based tests to detect TB, especially for target groups with sputum scarcity. In recent years, other biological samples such as urine, blood, exhaled breath are being tested (Peter et. al, 2010).
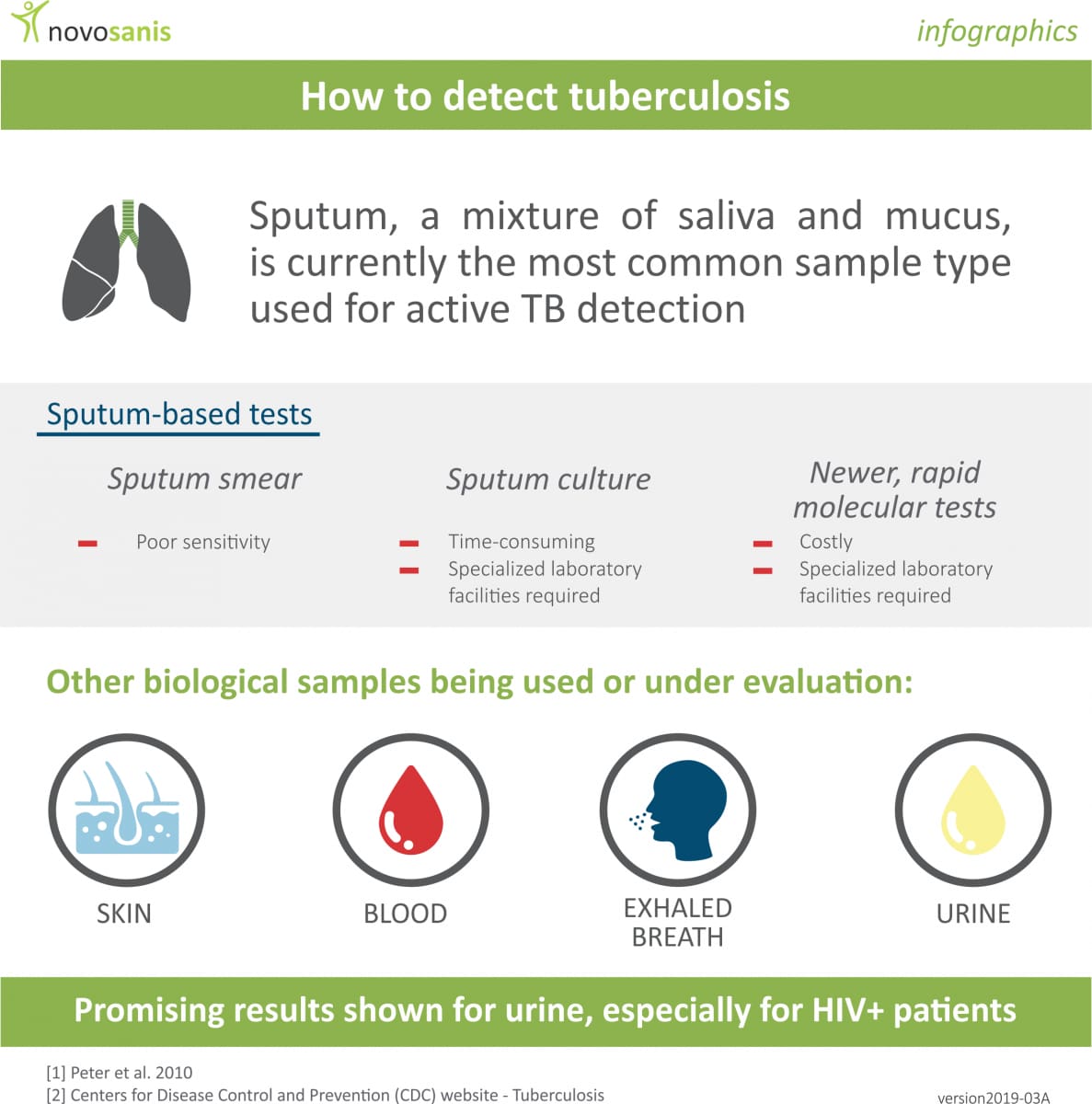
Urine in particular has shown great promise. This sample type is easily obtainable from all age groups, offers simple processing and storage abilities, can quickly be examined and has low infection risk for healthcare professionals during sample collection (Peter et. al, 2010).
Several studies have identified the possibilities of detecting MTB bacteria in urine. For example, mycobacterial lipoarabinomannan (LAM) is present on bacteria cell walls and is released from metabolically active or degenerating cells in people with active TB. Current literature demonstrates LAM assays to be effective and allow improved sensitivity for TB detection in individuals coinfected with HIV. However, currently the method is not suitable to screen for TB in all populations due to lower sensitivity compared to other used technologies (Peter et. al, 2010).
While more research is needed to make stronger recommendations for clinical practice, early evidence, supported by WHO, suggests that urine has the potential to improve TB detection, especially for specific target groups. Finding other biomarkers in urine for TB or understanding whether specific fragments of urine, such as first-void or midstream samples perform better in TB detection are also interesting areas to further explore.
References:
- Peter J, Green C, Hoelscher M, Mwaba P, Zumla A, Dheda K. Urine for the diagnosis of tuberculosis: current approaches, clinical applicability, and new developments. Curr Opin Pulm Med. 2010 May; PubMed PMID: 20375787
- Tavares e Castro A, Mendes M, Freitas S, Roxo PC. Diagnostic yield of sputum microbiological analysis in the diagnosis of pulmonary tuberculosis in a period of 10 years. Rev Port Pneumol (2006). 2015 Jul-Aug; PubMed PMID: 25926254.
- World Health Organization (WHO). High-priority target product profiles for new tuberculosis diagnostics: report of a consensus meeting. Geneva, Switzerland. 2014.
- World Health Organization (WHO). Global Tuberculosis 2018 Report. 2018.
- World Health Organization (WHO) website - Tuberculosis
